Introduction and objective
Impact of lymph node dissection (LND) at the time of radical nephrectomy (RN) for renal cell carcinoma (RCC) remains contentious, though the prognostic benefit in advanced renal masses has been well described. Prior reports have grouped heterogeneous histologies in their analyses. We sought to assess the impact of LND during RN for various histologies in kidney cancer.
Methods
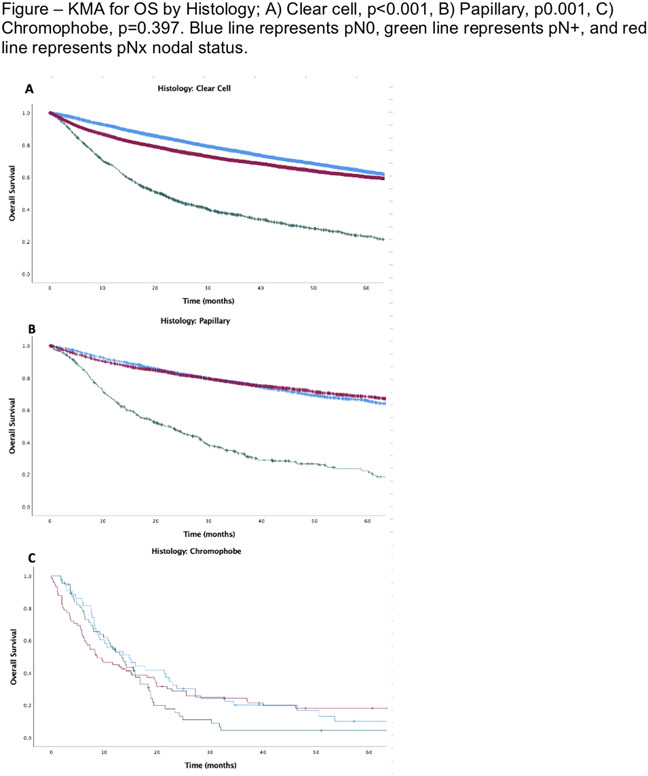
The National Cancer Database was queried between 2004-2015 for patients with clinical stage T2 and T3 RCC that underwent RN with and without LND. Descriptive analyses and multivariable regression (MVA) were performed to elucidate factors associated with overall survival (OS) for differing RCC histologic type. Kaplan-Meier analyses (KMA) were used to determine the survival based on LND and nodal status on OS based stratified by RCC histology.
Results
A total of 79,674 patients were analyzed by histologic type. pN1 was associated with worsened OS for NOS (OR 4.8, p<0.001), clear cell (OR 4.2, p<0.001), papillary (OR 4.0, p<0.001), and sarcomatoid (OR 3.2, p<0.001) RCC. Chromophobe (p=0.846) and cyst-associated (p=0.74) RCC had no association between pN1 and OS. pNx, when compared to pN0, was associated with worsened OS in NOS (OR 2.0, p<0.001), clear cell (OR 1.2, p<0.001); and was not associated with OS in papillary (p=0.253), chromophobe (p=0.48), cyst-associated (p=0.112), and sarcomatoid (p=0.113) histology. KMA Comparisons of 5-year OS between pN0, pN1 and pNx yielded: NOS 37%, 10% and 22% (p<0.001), clear cell 42%, 14%, and 42% (p<0.001), papillary 44%, 10%, and 48% (p<0.001), chromophobe 10%, 8%, and 14% (p=0.397), cyst-associated 44%, 0%, and 55% (0.891), and sarcomatoid 15%, 5%, and 13% (p<0.001), respectively (Figure).
Conclusions
Prognostic benefits of LND at time of RN for cT2-3 RCC vary by histologic subtype suggesting differences in underlying tumor biology. Clear cell, papillary, and NOS histology demonstrates prognostic benefits with LND, while chromophobe, cyst-associated, and sarcomatoid histology were not associated with benefit with LND. Histology, whether suspected or confirmed by biopsy, may be considered when deciding on performing LND in T2-T3 RCC. Further investigation is requisite.