Introduction and objective
The impact of open or minimally invasive surgery (either laparoscopic or robotic approach) on survival and disease recurrence in the management of non-metastatic renal cell carcinoma (RCC) remains uncertain. In this cohort study we assessed the impact of surgical approach on survival and on site-specific risk of first metastasis.
Methods
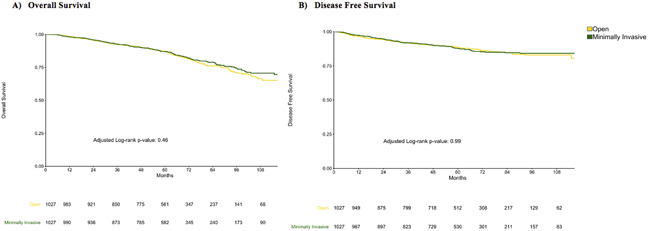
We used the RECUR database, a retrospective multi-institutional database of men diagnosed with RCC and submitted to renal surgery. We selected patient with pT1-3N0M0 RCC, and after propensity score matching (1:1 ratio, matching for age, year of surgery, gender, clinical size and pathological T stage surgical) a for open vs. minimally invasive surgery, either laparoscopic- or robot-assisted, the impact of surgical modality on overall survival (OS) and Progression-free Survival (PFS, including both distant or local recurrence) were assessed by use of Kaplan-Meier and multivariable Cox regression analyses. Site-specific risk of first recurrence, i.e. local recurrence or abdominal, thoracic and uncommon sites metastasis, was investigated by use of competing risk regression and cumulative incidence curves. In case of local recurrence propensity score matching model was implemented with surgical technique (partial vs. radical nephrectomy)
Results
After matching, 1027 patients in open and 1027in minimally invasive surgery were included in the study. After a median follow up of 62 months, 124 patients in open and 127 in minimally invasive group developed local recurrence and/or distant metastsis; no differences were found in terms of OS (HR 0.88; 95% confidence interval [CI] 0.71-1.04; p=0.24) and PFS (HR 1.05; 95%CI 0.81-1.35; p-value=0.73) between the two groups. A higher risk of local recurrence (sHR 2.65; 95% CI 1.42-4.97; p-value 0.002) and uncommon site metastases (sHR 1.6; 95 CI 1.02-2.52; p-value 0.042) was found for minimally invasive surgery.
Conclusions
No differences were found in terms of OS and PFS between open and minimally invasive surgery. However, the risk for local recurrence and uncommon metastases was statistically higher for minimally invasive surgery. Given the overall low risk of recurrence, careful surveillance is the best management option for most patients.