Introduction and objective
While partial nephrectomy (PN) is the preferred treatment modality for small renal masses, percutaneous cryoablation (PCA) has emerged as an acceptable alternative with favorable outcomes. However, there is a deficit of long-term, high-quality data comparing the two techniques. We reviewed long-term oncologic outcomes following PN and PCA for renal masses utilizing a propensity score matching method.
Methods
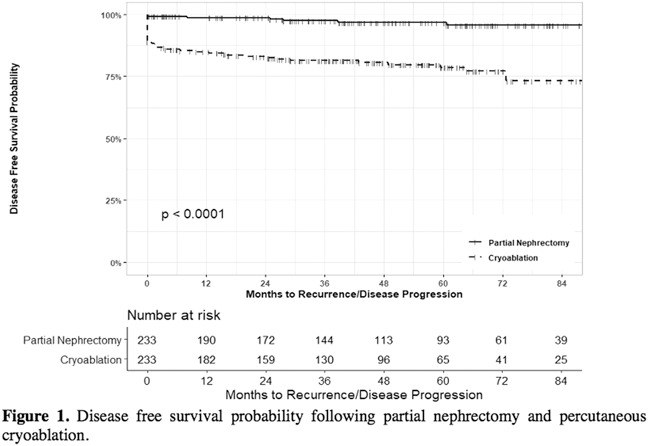
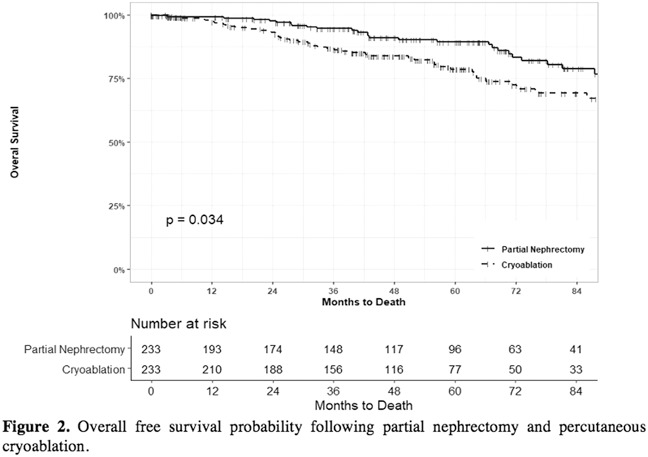
A total of 940 patients with renal masses treated with PCA or PN between 2005 and 2016 were identified within our prospectively maintained institutional database. Demographic and clinical variables and oncologic outcomes were assessed. Two hundred and thirty-three patients who underwent PN were propensity-score matched 1:1 to 233 patients who underwent PCA. Patients were matched based on demographics, Charlson Comorbidity Index (CCI), and tumor characteristics, with exact matching performed for nephrometry score. Disease-free survival (DFS) and overall survival (OS) were estimated using the Kaplan-Meier method.
Results
There were no statistically significant differences in sex, body mass index, tumor size, or nephrometry score between the cohorts. Mean patient age was 65.3±9.5 years in the PN and 68.1±10.5 years in the PCA cohort (p=0.002). Twelve percent of patients undergoing PN and 20.6% of patients undergoing PCA had CCI ≥4 (p=0.045). Median follow-up was 48.0 months for PN and 47.9 months for PCA. Five-year DFS was 96.7% and 78.5% for PN and PCA, respectively.
Conclusions
We report one of the largest propensity score matched analyses to date comparing long-term oncologic outcomes of PN and PCA. In our institutional experience, PCA has acceptable oncologic outcomes compared with PN when accounting for patient and tumor characteristics. A shared decision-making approach should be taken when choosing a treatment strategy.