Background
Despite recent advances in the treatment of clear cell RCC, there is a paucity of data to guide management of nccRCC due to the heterogeneity and rarity of these tumors. The clinical activity of combination therapies (including IO-IO, IO-VEGF, VEGF-mTOR) in subtypes of advanced nccRCC is unknown.
Methods
In this multicenter retrospective analysis, we evaluated the efficacy of combination systemic therapies in patients with nccRCC. Eligible patients included those with nccRCC as determined by local genitourinary pathology review and receipt of one of three combination regimens during any line treatment (IO-IO, IO-VEGF, mTOR-VEGF). The primary endpoint was objective response rate (ORR) assessed by investigator review. Secondary endpoints were progression- free survival (PFS), disease control rate (DCR), and overall survival (OS).
Results
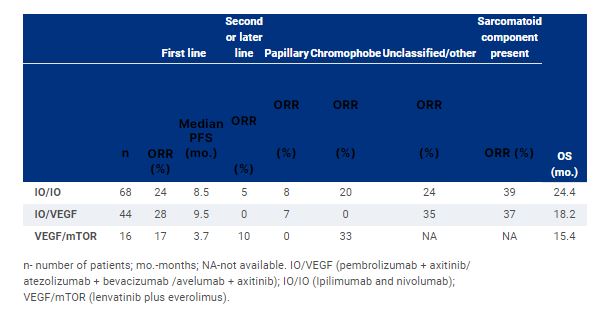
Among 128 included patients, median age was 57 years; 66% were male and 65% white. Histologies included papillary (37%), unclassified (33%), chromophobe (16%), translocation (9%), and other (5 %). Among all patients, 69% had prior nephrectomy; 80% were IMDC intermediate/poor risk; 20% had sarcomatoid and/or rhabdoid differentiation, 27% and 29% had liver and bone metastasis respectively and 63% received combination treatment as first line. Comparison of outcomes based on treatment regimen, line of treatment and subtype is shown in the table. Median PFS and OS were longer with IO/IO and IO/VEGF compared to VEGF/ mTOR at 8.5, 9.5 and 3.7 months and 24.4, 18.2 and 15.4 months respectively.
Conclusions
Antitumor activity was observed with novel combinations in nccRCC in both frontline and later line setting. Optimal management of nccRCC remains an unmet need and prospective data is warranted to guide treatment selection for this population.