Introduction and objectives
The aim of the study is to compare oncologic outcomes of partial nephrectomy (PN), radiofrequency ablation (RFA) and cryoablation (Cryo) and to examine the potential benefit of ablative techniques compared to PN.
Methods
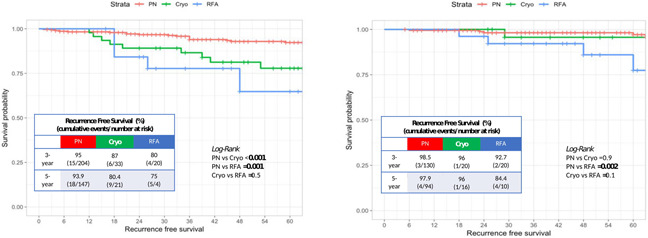
We retrospectively evaluated data from 665 (81.4%), 68 (8.3%) and 83 (10.3%) patients with cT1a renal cell carcinoma (RCC) who underwent laparoscopic or robotic PN, percutaneous RFA and Cryo at two tertiary centers, respectively. Younger patients were scheduled for PN. Ablative techniques were recommended in older patients at higher risk of complications. Kaplan-Meier curves depict recurrence-free survival (RFS) rates in the overall population and after stratifying according to tumor’s histology (namely, clear cell RCC and non-clear cell RCC) and size (namely<2 cm and 2-4 cm). Multivariable Cox regression model was used to identify predictors of recurrence. Cumulative-incidence plots evaluated disease recurrence and other causes of mortality (OCM).
Results
Patients referred to PN experienced higher rates of postoperative complications (30.7%) compared to men referred to RFA (10.3%) and Cryo (13.3%; p<0.001), with no significant difference for high grade complications (p=0.6). Patients referred to PN experienced higher RFS rate compared to those treated with RFA and Cryo at 60-month in the overall population (96.4% vs. 79.4 % and 87.8%), in patients with clear cell RCC (93.3% vs 75% and 80.4%) and in those with tumor of 2-4 cm (97.3% vs 78% and 84.4%; all p≤0.01). In patients with non-clear cell RCC and with tumor < 2 cm, PN showed higher RFS rate at 60-month as compared to RFA (97.9% vs 84.4% and 95.1% vs 78.1%, respectively; all p≤0.02). At multi-variate analysis, ablative techniques (RFA [HR=4.03] and Cryo [HR=3.86]) were independent predictors of recurrence (all p<0.03). At competing risks analysis, recurrence rate and OCM were 7.3% and 1.3% vs 25% and 7.2% vs 19.9% and 19.9% for PN, RFA and Cryo, respectively.
Conclusions
PN and Cryo showed similar RFS rates in patients with non-clear cell RCC and with renal mass < 2 cm, therefore, biopsy of renal mass could be useful to select patients before renal ablation, to avoid to ablate tumors at higher risk of recurrence.
Source of Funding
None