Introduction and objectives
Renal artery pseudoaneurysm (RAP) after partial nephrectomy is uncommon but a potential life-threatening complication. The aim of the study is to investigate the incidence of RAP after RaPN and identify the predictive factors.
Methods
We reviewed our institutional robotic-assisted partial nephrectomy (RaPN) database conducted from December 2009 to August 2020. Renal artery pseudoaneurysm (RAP) was diagnosed by computed tomography angiography (CTA) for patients who were suspected of having RAP clinically. Patients who had RAP after RaPN were compared with other patients who did not have RAP. Patients’ demographic data, tumors’ characteristics, and operative outcomes were evaluated. Statistical analyses were used to identify the predictive factors of RAP after RaPN.
Results
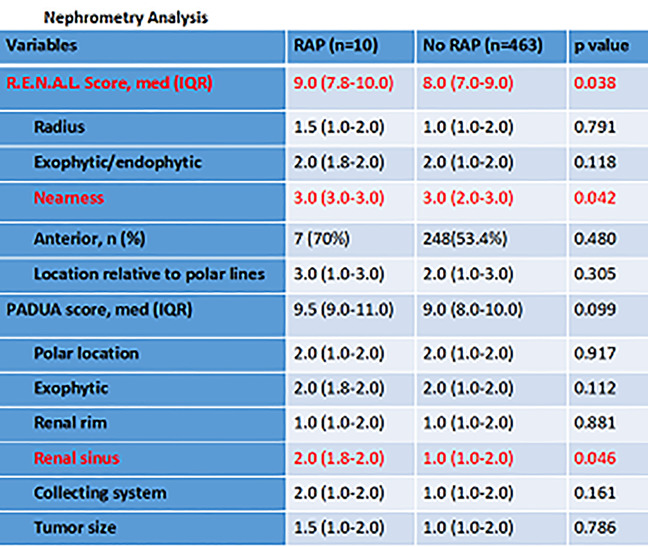
A total of 473 patients who underwent RaPN was reviewed, and 10 patients (2.1%) developed RAP median of 10 days (interquartile range: 6 – 14.5 days) after surgery. Most those patients experienced gross hematuria and were diagnosed by CTA. No patients had recurrent RAP during follow-up after treatment (8 patients underwent embolization, 1 patient underwent exploratory laparotomy, and 1 patient underwent observation). No difference was found in tumor size, total preoperative aspects and dimensions used for an anatomical (PADUA) scores, total operative time, warm ischemia time, blood loss, intraoperative blood transfusion rates between patients who had RAP versus controls. However, higher total higher R.E.N.A.L Nephrometry Score (median 9.0 versus 8.0, p=0.038), more renal sinus involvement in PADUA score (median 2.0 versus 1.0, p=0.045) and longer postoperative hospital stays (median 6.0 days versus 5.0 days, p=0.014) were noted in the patients who had developed RAP postoperatively. Besides, more proportion of patients who had 3 points N score (nearness to renal sinus or collecting system) in R.E.N.A.L score in RAP group, which reached statistically significance (p=0.042).
Conclusions
The incidence of RAP is rare (2.1%). The occurrence of RAP is associated with higher R.E.N.A.L Score, and longer postoperative hospital stays. In nephrometry analysis, nearness of tumor to sinus or renal sinus involvement is associated with occurrence of RAP.
Source of Funding
None