Introduction and objective
Performing image-guided biopsy of incidental small renal masses (SRMs) pre-treatment to minimise overtreatment of benign renal masses is advocated. This study aims to assess the trends and potential factors influencing the decision to perform image-guided biopsy before cryoablation treatment.
Methods
From December 2014 to October 2020, patients with T1N0M0 SRMs undergoing percutaneous cryoablation from 14 European institutions within the European Registry For Renal Cryoablation (EuRECA) were included for the retrospective analysis. The trends of performing image-guided biopsy as a separate session before cryoablation of SRMs were analysed over time, and the potential factors influencing the decision to perform image-guided biopsy before treatment were analysed using multivariate logistic regression model.
Results
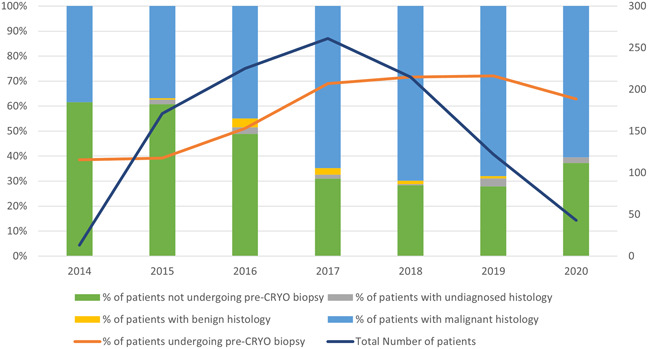
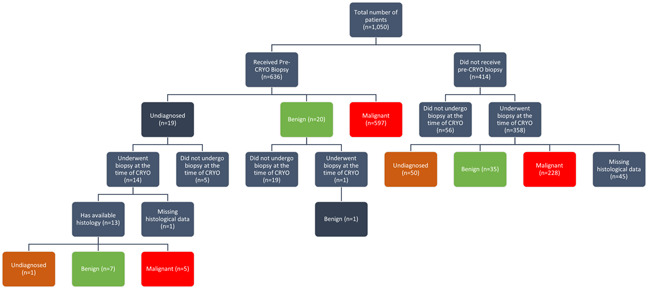
1,050 patients were evaluated. The use of pre-cryoablation biopsy has significantly increased from 39% (67/171) in 2015 to 72% (88/122) in 2019 (p <0.001; figure 1). Rates of undiagnosed histology and benign histology is significantly higher in patients undergoing biopsy at the time of treatment (16% [50/313] vs 0.16% [1/636], p <0.001; Figure 2). For every 4.5 patients receiving pre-cryoablation biopsy, one less patient receives cryoablation treatment for a non-malignant renal tumor. Aged 70-79 (OR 0.53, 95% CI 0.29-0.96), 80-89 (OR 0.47, 95% CI 0.24-0.92), obesity (OR 0.73, 95% CI 0.55-0.98) and having a solitary kidney (OR 0.40, 95% CI 0.27-0.61) are three patients' factors associated with less likelihood of pre-cryoablation biopsy (p 1 (OR 2.11, 95% CI 1.54-2.88) are factors associated with higher likelihood to have received a pre-cryoablation biopsy (p <0.05).
Conclusions
Pre-cryoablation biopsy should be advocated as it is more likely to lead to confirmatory histological diagnosis than biopsy at the time of cryoablation, thus reducing overtreatment of non-malignant SRMs.