Introduction and objective
Nonhereditary Bilateral Multifocal (BMF) Type 1 Papillary Renal Cell Carcinoma (pRCC) represents a subtype of renal cancer which exists in the absence of a family history of RCC and without germline MET mutations. This patient population is at risk for recurrent renal surgeries, and potentially renal deterioration. Paucity of data exists surrounding management strategies, clinical and oncological outcomes, and active surveillance of these patients. We report our surgical experience with this unique cohort at the National Cancer Institute.
Methods
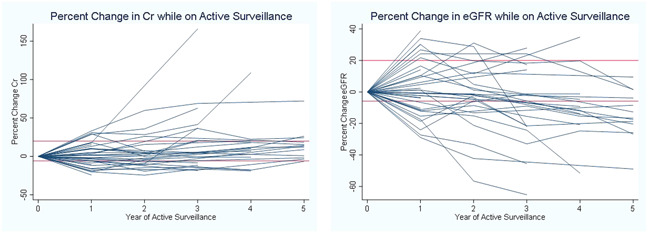
Patients with BMF pRCC, negative germline MET mutation and no family history evaluated at the National Cancer Institute from 2002 to 2020 were reviewed. Demographics, clinical presentation, tumor size, and renal functional outcomes were retrospectively analyzed. Patients were managed similarly to hereditary RCC, with active surveillance (AS) until the largest tumor is 3 cm, followed by multiplex partial nephrectomy when feasible. AS was defined as a visible kidney lesion on imaging with at least 6 months follow-up. Percent change creatinine and eGFR on active surveillance were evaluated.
Results
There were 77 patients with BMF pRCC and 129 surgical interventions. Median number of tumors per patient was 6. Five(6.5%) patients presented with metastatic disease (median tumor size 6.5cm), 1(1.3%) progressed to metastasis during follow up. No patients developed metastatic disease when their largest tumor was 3cm or less. At presentation, the median serum creatinine (Cr) =1.85 mg/dl, median eGFR=60. Thirty-eight patients were managed with AS (median 51 months). Median tumor size at enrollment on AS was 2.1cm. At the start of AS median Cr=1.23 mg/dl (1.01–1.47) and eGFR=62 (54–83). At the end of AS median Cr=1.24 mg/dl (1.13–1.53) and eGFR=62 (50–72). Percent change Cr from baseline on AS was 6.90% (-5.81–20.0), and eGFR was -9.07% (20.69–3.27). No patients developed metastatic disease on AS.
Conclusions
Nonhereditary BMF pRCC represents a unique entity. Despite presenting with renal impairment, this cohort had stable renal function during AS. AS until the largest renal tumor reaches 3 cm followed by nephron sparing surgery has acceptable oncologic outcome and is recommended.
Source of Funding
NIH Intramural Research Funding, NIH Medical Research Scholars Program, Foundation for the NIH